The 10-Year Health Plan: Reflections & Implications

The new 10-Year Health Plan outlines an ambitious vision to modernise care, bring services closer to home, and empower patients using technology and prevention.
The long-awaited plan carries significant weight. Since taking office, the Labour Government has described the NHS as being in a state of crisis, a claim reinforced by Lord Darzi's review, which identified a range of serious challenges. The plan reflects this message, stating clearly that the NHS must choose between reform or collapse.
However, one key question remains: can it deliver on its promises?
While the plan aims to improve health outcomes, it reads more like an NHS reform than a comprehensive cross-government health strategy. Closing the life expectancy gap will require much broader action beyond the health service, including addressing the underlying social and economic causes of poor health.
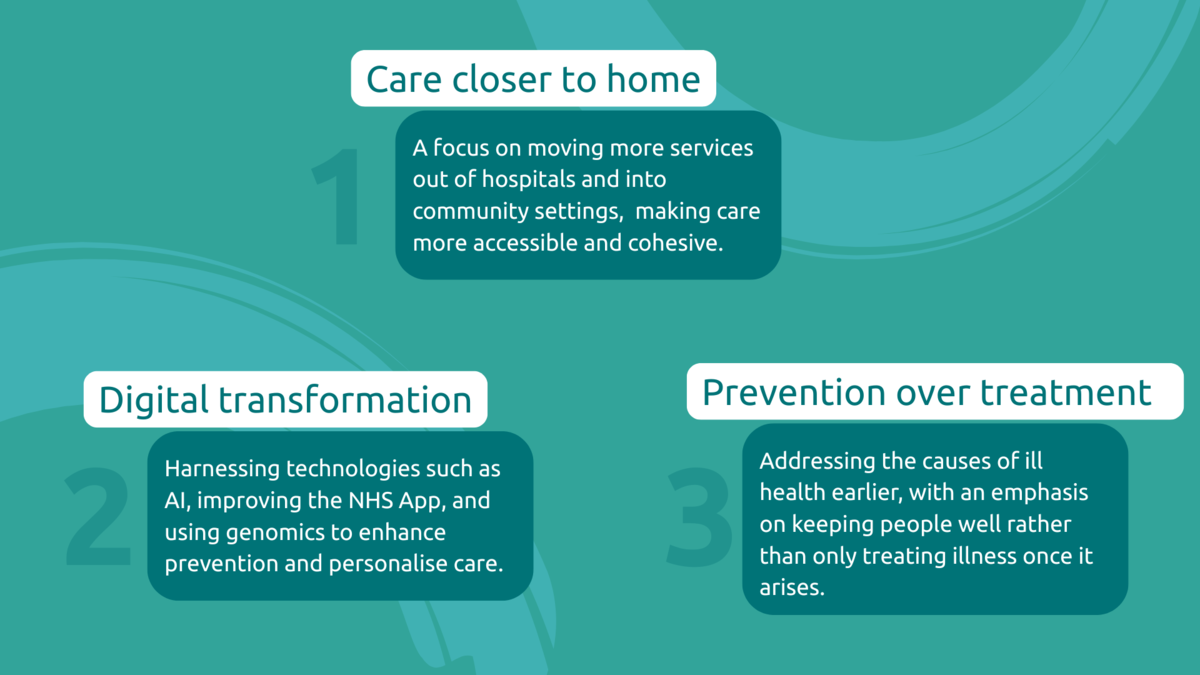
The plan is built around three big shifts:
What will change?
The plan outlines a range of structural reforms, new legislation and funding models.
Key changes include:
- A redesigned NHS App enabling patients to manage their care, self-refer to services, and use built-in translation services to access support in their preferred language
- Neighbourhood health centres in every community, starting with those facing the poorest health outcomes
- Greater investment in out-of-hospital services, such as GPs, mental health support, home-based care, and preventative health
- The integration of genomic data into NHS Health Checks to help detect risks earlier
- Innovation zones and targeted investment in cutting-edge technologies like AI scribes, wearable health monitors, and robotics
- A stronger emphasis on patient voice, with new measures to gather and respond to patient feedback in meaningful ways
The positives
The plan outlines several positive steps that could help put patients more firmly at the centre of their care. There is a clear commitment to making services more personalised, with better feedback systems and tools that support people to manage their health.
Improvements to the NHS App and the introduction of a single patient record have the potential to make access easier, reduce duplication, and ensure professionals have the information they need to offer cohesive support.
Importantly, the plan also recognises the need to do more for people who have been historically left behind.
Neighbourhood Health Centres will be rolled out first in areas with the poorest health outcomes. There is a focus on giving people more control over their care, which includes a commitment to ensure that 95% of people with complex needs have a personalised care plan in place by 2027.
Additionally, the Government has pledged to increase the number of people with Personal Health Budgets, aiming to reach one million people by 2030 and make this a universal offer by 2035.
Our concerns
This is not a true cross-government health plan
The primary focus of the plan is reforming the NHS.
While the NHS forms an integral part of the UK's health system, there are significant gaps in the social determinants that contribute to the overall health of people living in the UK.
The plan focuses on prevention as one of its three main pillars, citing initiatives, pilots and legislation to reduce health implications related to smoking, pollution, obesity, alcohol and genetic factors.
Although these factors are, of course, drivers of many health issues, what the plan doesn't acknowledge is the key socio-economic factors contributing to poor health and lower life expectancy, such as poverty, inadequate housing, and care entry rates.
Neglect of social care
Strikingly, there is limited focus on integrating the health plan with the wider social care system, despite the crucial role that social care plays in alleviating pressure on the NHS.
Additionally, there is no mention at all of reform to NHS Continuing Healthcare, a system that many find confusing and difficult to navigate.
While the plan states that the Better Care Fund will be reformed, it offers no details about how or when this will happen. Meanwhile, the Casey Commission on Care and Support is not expected to report until 2028, leaving a major piece of the health and care puzzle unresolved for years to come.
The risk of digital exclusion
The plan puts the NHS App front and centre of many of the reforms, intending on streamline services and empower patients.
However, this digital takeover risks excluding those without access to technology or the necessary skills to use it, particularly older individuals and those living in digital poverty. People with disabilities or complex needs may also face greater pressure to self-manage and navigate digital tools, making it harder to access the support they need without tailored assistance.
Concerns around AI
While AI tools like scribes and apps may streamline some processes, they cannot compensate for outdated IT systems and clunky infrastructure still in place across much of the NHS. Without clear communication on data privacy and safeguards, there is also a risk of public mistrust and misuse.
The plan introduces the use of AI in complaints handling procedures: a tool is already being piloted on the Federated Data Platform, with plans to expand in 2025–26. Complaints handling is deeply personal, and many people turn to services like PALS after experiencing distressing or traumatic care.
Replacing human contact with AI risks dehumanising the process and undermining trust at a time when people most need to feel heard and supported.
Mental health gets piecemeal attention
Although the plan proposes small-scale actions to target mental health, there is seemingly no clear integration of mental health into wider system reforms or funding changes.
It remains unclear how new payment models will impact mental health providers, particularly those still operating under outdated block contracts. This lack of clarity is concerning, especially as the standalone Mental Health Strategy and the Major Conditions Strategy were both scrapped in favour of the Health Plan.
Furthermore, given the growing number of people claiming disability benefits due to mental health conditions, as highlighted in the Universal Credit Bill, it is troubling that there is little focus on reforming the mental health system entirely to support this growing need.
Weak action on health inequalities
The plan sets a low ambition for tackling health inequalities, stating that by the end of its ten-year period, it will have only begun to narrow these gaps and restart progress on life expectancy.
Given the stark and growing health disparities across England, this falls far short of what is needed. The scale of inequality demands urgent and transformative action across both the health and social care systems, not a slow start over a decade.
Patient payments raise red flags
The plan outlines that payments may be withheld from providers if patients feel dissatisfied with their care.
While giving patients more say over whether full payments are released to providers sounds empowering, we are concerned about potential ethical and practical implications. We do not want to see this approach end up encouraging data manipulation, damaging trust between patients and providers, or undermining a culture of learning.
There is also a lack of clarity on how feedback will be gathered in ways that meaningfully include disabled people, neurodivergent individuals, and those with complex needs, groups who may face barriers in communicating their experiences or whose care outcomes may not be easily captured by standard satisfaction metrics.
There is a risk this model could shift focus from genuine improvement to performance management, with unintended consequences for care quality and staff wellbeing.
Implications for our service users
While the plan promises better support for people with disabilities and a reduction in health inequalities, there is little detail on how these outcomes will be achieved in practice.
For children and families, the intention to improve transitions into adult services is welcome; however, it lacks the clarity needed to ensure meaningful change.
The increased focus on digital tools means individuals with complex needs may be expected to manage their care plans online. This could place a significant burden on those who are digitally excluded or rely on unpaid carers.
Neighbourhood care and closer-to-home services undoubtedly offer many potential benefits, but reliance on telephone or digital appointments may not be appropriate or accessible for everyone.
Without careful consideration, this shift risks overlooking safeguarding concerns and could create new barriers to care for those who are most in need.
What's needed
To truly improve health outcomes, there must be a stronger focus on tackling the root causes of inequality, such as housing, poverty, and prevention. These issues cannot be resolved by the NHS alone.
Social care and mental health must be treated as equal priorities, placing clear reform plans and sustainable funding at the forefront of the health plan. Meaningful change will come from genuine cross-sector collaboration, not just NHS-led initiatives.
Success also depends on proper investment in people, services, and basic infrastructure. Ultimately, digital strategies must be inclusive and accessible to everyone, with targeted support for those who are most likely to be left behind.
Stay informed about our work by:
Signing up for our campaign updates
Checking our website news





